Preparing for End of Life
Early discussions with a resident and their family/carer, acknowledges the impact of their life limiting conditions and inevitable decline. Documenting what the resident would like at the end of life, can help to avoid conflict and rushed decision making.
Advance Care Planning enables an individual to make plans about future health care. It provides a direction for a family and health care team when the individual is no longer able to make and/ or communicate their choices.
Advance Care Planning Australia is a national project funded by the Australian Government Department of Health and Aged Care. This project provides resources to enable individuals to make the best choices for their future health and care. General practitioners and aged care teams play a key role in Advance Care Planning so it’s important for them to have a good understanding of what advance care planning is and what’s involved in the advance care planning process.
Advance Care Planning Australia provides training and education for aged care workers to improve their knowledge, skills and confidence when having advance care planning conversations. Resources include a range of online courses, workshops, webinars and information sessions as well as resources for diverse cultural populations.
Starting the conversation about advance care planning is an important first step in ensuring an individuals preferences for future care are known and respected. Where the conversation is taking place with someone who has difficulty with decision making, accessing Palliative Care Victoria’s Dignified and Respectful Decisions resources can be helpful.
For further information:
- End of life Directions in Aged Care (ELDAC) Factsheet
- Resources for diverse cultural populations
- Advance care planning forms
- Resources for people who lack capacity to undertake Advance Care Planning;
- Northern Health Advance Care Planning Tools
- Appointment of medical treatment decision maker (health.vic.gov.au)
- Advance care directive for adults (health.vic.gov.au)
- Aged Care Quality Standards and Glossary – Final Draft – Nov 2023 (health.gov.au)
- Office of the Public Advocate
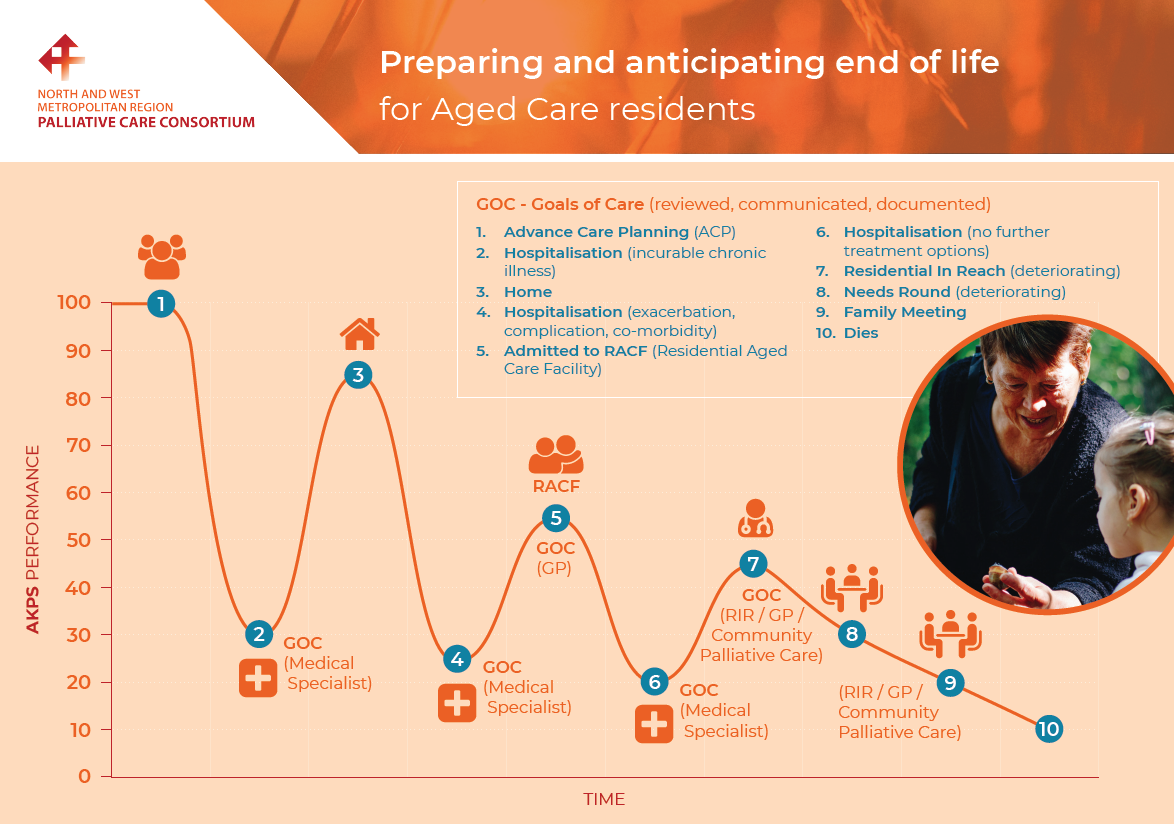
Goals of Care describe the medical treatments a resident will receive that incorporate their wishes and preferences. When a resident is no longer receiving curative treatment, Goals of Care can help to ensure they receive appropriate interventions and are not subjected to burdensome or futile treatments. They should be identified and documented by the resident’s medical specialist or General Practitioner in consultation with the resident and their family.
Useful links providing information about Goals of Care include:
- palliAGED Goals of Care overview
- Victorian Department of Health Goals of Care information
- Australian Commission on Safety and Quality in Health Care
Goals of Care should be identified and documented by the residents medical specialist or General Practitioner in consultation with the resident and their family/carers. They are informed by open, honest and realistic discussion around end-of-life care and should be reviewed and updated as the resident’s status changes.
Click here for Advance care planning and goals of care YouTube video (9.29 minutes). This video provides a guide for Residential Aged Care staff when discussing advance care planning and goals of care with family and carers.
Conducting a family meeting can be a useful way to provide information in response to a family’s questions and concerns and to establish Goals of Care. This trajectory graph below provides guidance on when to establish and review Goals of Care. Early identification of deterioration and regular review of Goals of Care supports a peaceful and dignified death.
Safer Care Victoria has developed a generic care plan for the dying person. Click here for the link.
Family meetings are invaluable and one way in which the resident and their family can be involved, empowered and supported by the care team. Here are some helpful links:
Family meetings working with family
ELDAC resources: Talking with families
Family meetings are a proactive way of managing and planning care and should be considered:
- On admission of a resident to aged care
- When a life limiting condition is identified
- When discharge is planned from an inpatient setting
- As the resident’s condition changes
- As part of a referral to a specialist palliative care service
- When there is lack of agreement amongst family/carers regarding the plan of care